By Kathy Lester, JD, MPH | Updated November 9, 2015
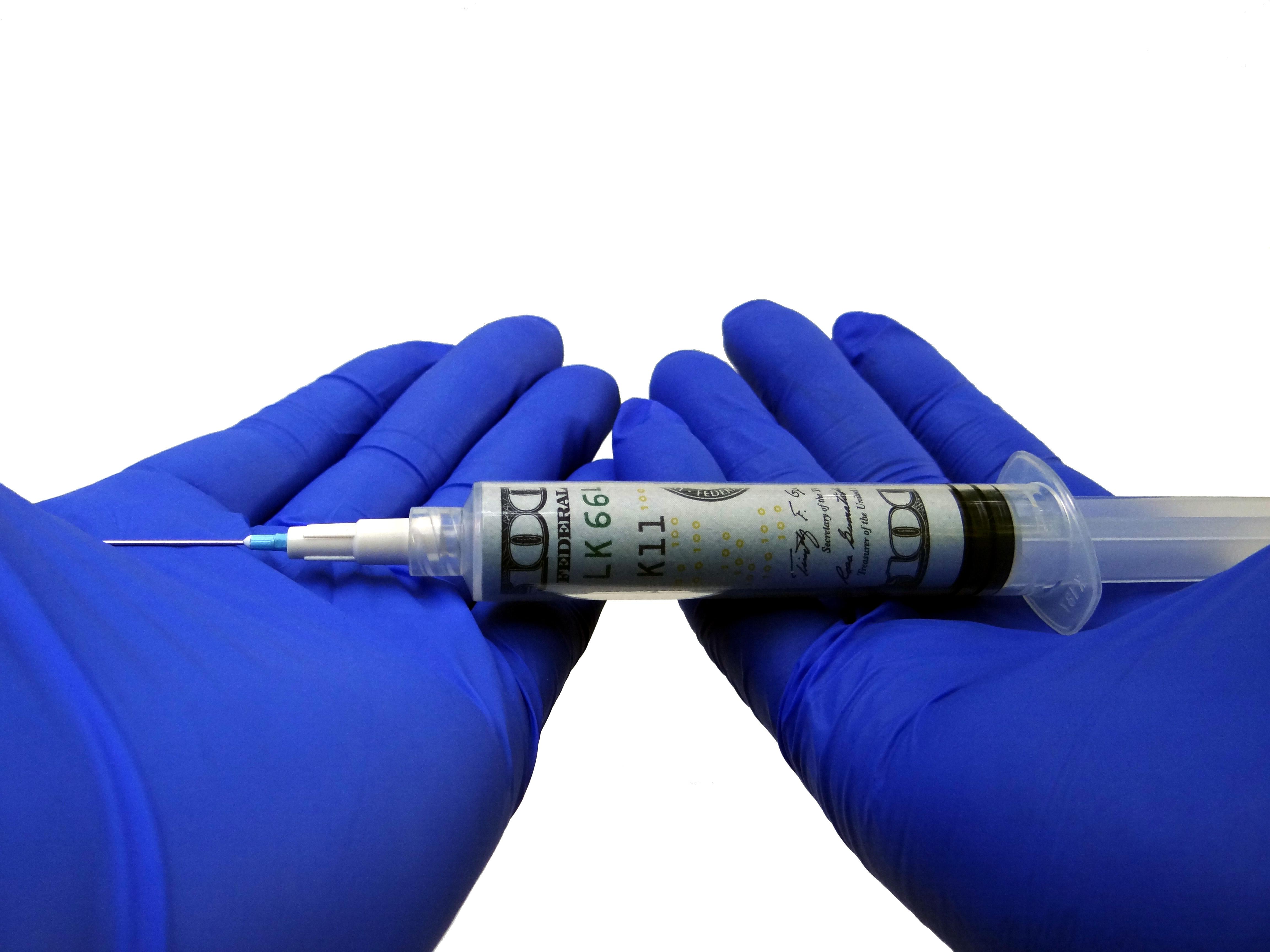
Tomorrow is in your hands today. This statement is especially true when we think about the evolution of ambulance services. Today, care once reserved for the hospital setting is now delivered at the scene, resulting in better patient outcomes. Yet, despite these advances, the Medicare payment system lags behind. Current rates are based upon a negotiated rulemaking process that did not take the cost of providing services into accounts. While many in the industry strive to further expand the delivery of high-quality care, the inflexibility of the current payment system makes it difficult to compensate the next generation of ambulance service providers appropriately.
To prepare for tomorrow, ambulances services must act today. The AAA has taken a leadership role by setting the groundwork needed to reform the payment system so that it recognizes the continued evolution of ambulance services. The two game changers are (1) designating ambulance suppliers as “providers” of care; and (2) implementing a federal data collection system.
“Emergency care has made important advances in recent decades: emergency 9-1-1 service now links virtually all ill and injured Americans to immediate medical response; organized trauma systems transport patients to advanced, lifesaving care within minutes; and advances in resuscitation and lifesaving procedures yield outcomes unheard of just two decades ago.”
–Institute of Medicine: Emergency Medical Services at a Crossroads (2007)
Provider Status
Being deemed a “provider” rather than a “supplier” is the first step toward recognizing the clinical component of ambulance services and appropriately incorporating ambulance services into the broader health care coordination and reform discussions.
Under current law, the term provider refers to hospitals, skilled nursing facilities (SNFs), outpatient rehabilitation facilities, home health agencies, ambulatory surgical centers, end-stage renal disease facilities, organ procurement organizations, and clinical labs. Durable medical equipment entities and ambulance services are designated as suppliers.
When ambulance services were first added to the Medicare benefit, the primary services provided were transportation. As noted already, transportation is only one component of the services provided. The deliver of health care services today make ambulances more like other Medicare providers than suppliers.
Achieving this designation is the first step toward having the federal government recognizing the value of the health care services provided by ambulances.
Cost Collection
The second game changer involves collecting cost data from all types and sizes of ambulances services in all areas of the country. Current Medicare rates are not based on cost. As the Government Accountability Office has recognized in two separate reports, these rates do not cover the cost of providing services to beneficiaries. While the Congress has extended the ambulance add-ons year after year, the lack of a permanent fix makes it difficult to plan. There is also the risk of the add-ons not being extended at some point. In addition, the rates take into account only at the most general level the health care being provided.
In the American Taxpayer Relief Act (ATRA), the Congress required the Centers for Medicare and Medicaid Services (CMS) to issue a report evaluating the ability to use current hospital cost reports to determine rates and also to assess the feasibility of obtaining cost data on a periodic basis from all types of ambulance services. Knowing of the strong Congressional interest in obtaining additional cost information, the AAA began working with The Moran Company (a consultant organization with expertise in Medicare cost reporting) to develop recommendations as to how cost data could be most efficiently and effectively collected. The AAA shared these recommendations with CMS and the contractor developing the report. The final report, released in October, supports the AAA’s work and states:
Any cost reporting tool must take into account the wide variety of characteristics of ambulance providers and suppliers. Efforts to obtain cost data from providers and suppliers must also standardize cost measures and ensure that smaller, rural, and super-rural providers and suppliers are represented.
The next step in the process is to provide CMS with direction and authority to implement the AAA’s cost survey methodology. In brief, the methodology would:
- Require all ambulance services to report to CMS demographic information, such as organizational type (governmental agency, public safety, private, all volunteer, etc), average duration of transports, number of emergency and nonemergency transports. CMS would use this data to establish organization categories so that the data collected aligns with the type of organization providing it.
- Require all ambulance services to report cost data, such as labor costs, administrative costs, local jurisdiction costs, through a survey process. During any survey period, CMS would identify a statistically valid sample of ambulance services in each category to be surveyed. These services would have to provide the data or be subject to a five percent penalty. Those ambulance services that provide data will not be asked to do so again until every service in its organization category has submitted the data.
As part of this process, the AAA has begun developing a common language for reporting these data. This work will ensure that the information is collected in a standardized manner. The AAA will also provide assistance to services that may need extra help in completing the surveys.
This information can then be aggregated and used to evaluate the adequacy of Medicare payments and support additional coverage policies. Most importantly, it will allow policy-makers, the AAA, and other stakeholders to reform the current Medicare ambulance payment system so that it incorporates the health care services currently being provided and those that will be in the future.
Conclusion
In order to be prepared for the reimbursement structures of tomorrow, ambulance services need to be designated a providers and recognized for the health care they provide. They also need to participate in a standardized cost collection program that will provide accurate data in the least burdensome way possible. The AAA is leading the effort to help ambulance services prepare for tomorrow.